The TCR coverage upcoming!





Historically, mechanical complications following acute myocardial infarction have been associated with very high morbidity and mortality. Despite their incidence plummeted with the advent of acute reperfusion therapy, such as thrombolysis and percutaneous coronary intervention, contemporary data on the outcomes of patients who develop such ominous complications are scarce. CAUTION study (NCT03848429), a retrospective, international, multicenter study aimed at evaluating the survival and postoperative outcomes of patients undergoing cardiac surgery for post-infarction mechanical complications. The recent publications from this registry, CAUTION PMR study (DOI: 10.1093/ejcts/ezab469) and CAUTION VSR study (DOI: 10.1001/jamanetworkopen.2021.28309), revealed an early mortality of 24.8% and 40.4% for subjects underwent surgical treatment for post-infarction papillary muscle rupture (PMR) and VSR (ventricular septal rupture), respectively. In light of this, further efforts of the health community should be directed toward improving therapeutic measures in an attempt to improve in-hospital survival of these critical subgroups of patients. Furthermore, publications investigating the long-term outcomes of patients undergoing surgery for post-infarction mechanical complications are warranted.
Background
Historically, impaired glucose metabolism has been associated with early and late complicated clinical outcomes after cardiac surgery. Such a condition, however, is not specific to subjects with diabetes mellitus and involves larger patient population.
Methods
Databases were screened (January 2000-December 2020) to identify eligible articles; studies, which evaluated the association between preoperative metabolic status, as assessed by glycosylated hemoglobin (HbA1c) levels, and clinical outcomes were considered. The studies were stratified in thresholds by baseline HbA1c level (lower vs higher).
Results
Thirty studies, involving 34,650 patients, were included in the review. In a meta-analysis stratified by HbA1c levels, early mortality was numerically reduced in each threshold comparison and yielded the highest reductions occurred when <5.5% vs >5.5% HbA1c levels were compared [Risk Ratio (RR) 0.39, 95% Confidence Intervals (CIs) (0.18-0.84), P=0.02]. Comparing higher HbA1c threshold values yielded comparable results. Late mortality was reduced with lower levels of HbA1c as well. Low pre-op HbA1c was associated with lowest risk of sternal wound infections [RR 0.50, 95% CI (0.32-0.80), p=0.003 and RR 0.53, 95% CI (0.39-0.70), p<0.0001] for comparisons of <7.5% vs >7.5% and <7.0% vs >7.0% HbA1c thresholds, respectively. Additionally, levels of HbA1c lower than 7% were associated with reduced hospital stay, lower risk of stroke/transient ischemic attack [RR 0.53, 95% CI (0.39-0.70), p<0.0001 and acute kidney injury: RR 0.65, 95% CI (0.54-0.79), p<0.0001].
Conclusions
Lower levels of HbA1c in patients undergoing cardiac surgery are associated with lower risk of early- and late mortality, as well as in the incidence of postoperative AKI, neurological complications, and wound infection, as compared to higher levels.; Keywords: diabetes mellitus; cardiac surgery; glycosylated hemoglobin; coronary artery bypass grafting.
full text (.PDF) available at JTCVS website
accompanying editorial (Breaking the Perioperative Glucose Control Barrier Is Like Breaking the Sound Barrier – It Takes a Team!) by Victor A. Ferraris
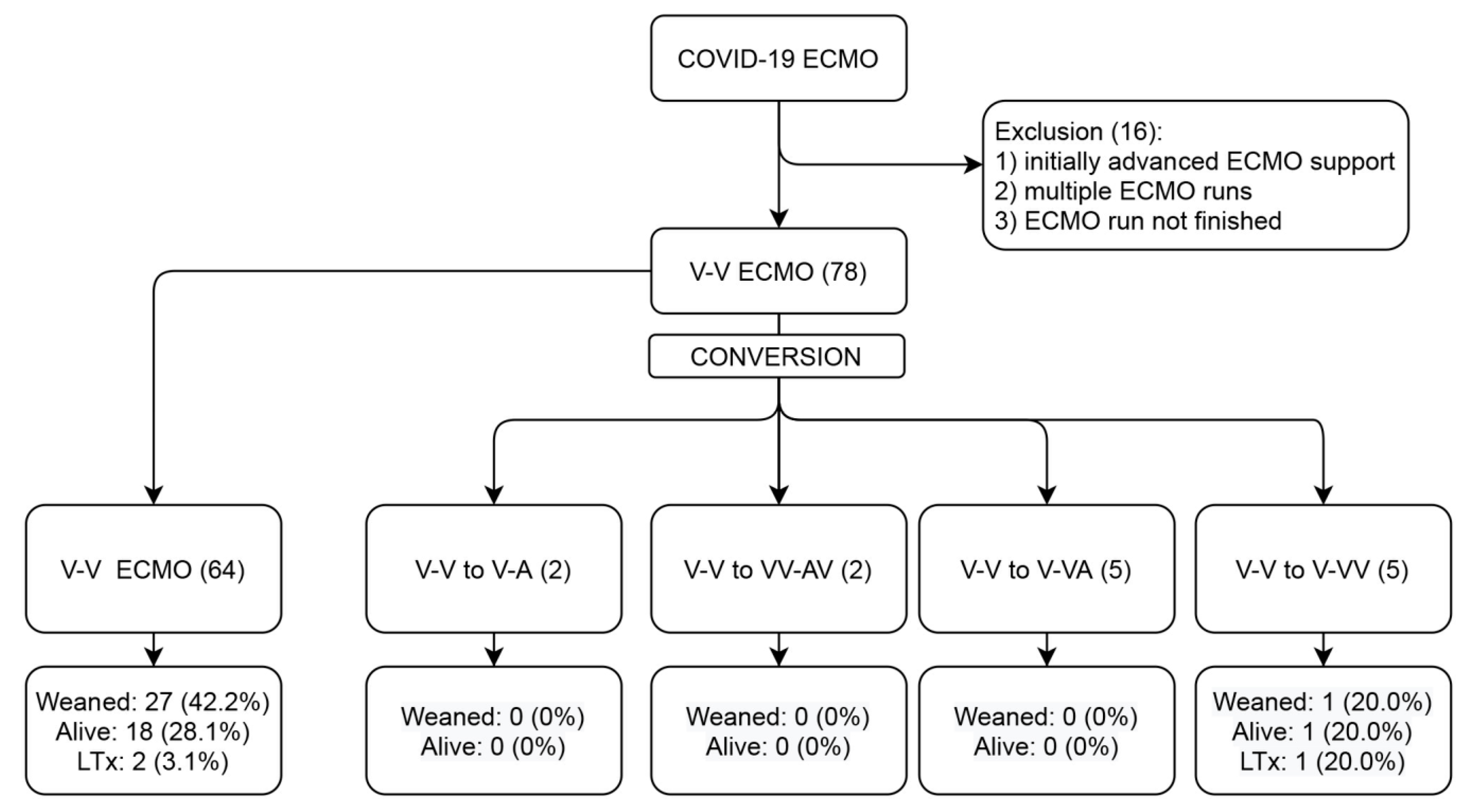
In SARS-CoV-2 patients with severe acute respiratory distress syndrome (ARDS), Veno-Venous Extracorporeal Membrane Oxygenation (V-V ECMO) was shown to provide valuable treatment with reasonable survival in large multi-centre investigations. However, in some patients, conversion to modified ECMO support forms may be needed. In this single-centre retrospective registry, all consecutive patients receiving V-V ECMO between 1 March 2020 to 1 May 2021 were included and analysed. The patient cohort was divided into two groups: those who remained on V-V ECMO and those who required conversion to other modalities. Seventy-eight patients were included, with fourteen cases (18%) requiring conversions to veno-arterial (V-A) or hybrid ECMO. The reasons for the ECMO mode configuration change were inadequate drainage (35.7%), inadequate perfusion (14.3%), myocardial infarction (7.1%), hypovolemic shock (14.3%), cardiogenic shock (14.3%) and septic shock (7.1%). In multivariable analysis, the use of dobutamine (p = 0.007) and a shorter ICU duration (p = 0.047) predicted the conversion. The 30-day mortality was higher in converted patients (log-rank p = 0.029). Overall, only 19 patients (24.4%) survived to discharge or lung transplantation. Adverse events were more common after conversion and included renal, cardiovascular and ECMO-circuit complications. Conversion itself was not associated with mortality in the multivariable analysis. In conclusion, as many as 18% of patients undergoing V-V ECMO for COVID-19 ARDS may require conversion to advanced ECMO support.
full text (.PDF) available at Membranes website
Dear Colleagues,
The pathophysiology of ischemic stroke is extremely complex, and despite advances in knowledge in this field, the understanding of the phenomena leading to acute cerebral ischemia and its consequences remains unknown. Previous experimental and clinical studies have shown that disturbances in blood coagulation and fibrinolysis, as well as an increased inflammatory response, play a significant role in the pathophysiology of ischemic stroke. For this reason, many researchers have described ischemic stroke as a thromboinflammatory disease. The interdependence between these phenomena, however, requires further research to clarify their role in the pathophysiology of ischemic stroke. Moreover, the relationship between these processes, the patient’s outcomes, and the effectiveness of the therapy used remains a mystery.
This Special Issue of Life aims to explore the role of hemostasis and inflammation, as well as the dependencies between them, in the pathophysiology, diagnosis, and treatment of ischemic stroke. I am pleased to invite you to submit a manuscript covering experimental and clinical research, as well as a systematic review and meta-analysis.
Prof. Artur Słomka
Guest Editor
Dear Colleagues,
Cardiac arrhythmias and, in particular, atrial fibrillation (AF), have become a burden in today’s aging society, and are often associated with numerous other comorbidities. While largely impacting heart function and quality of life, at the same time, the loss of proper cardiac contractility heralds the risk of systemic thromboembolism and stroke. On the positive side, new treatments are emerging for rhythm control, rate control and stroke prevention. Together with recent advancements in surgical and catheter ablation, we now have what seems to be a wide arumentarium to face rhythm disturbances. As also reflected in the recent 2020 ESC guidelines, cardiac ablation has gained higher recognition and its class of indication has been moved from IIa to I in many clinical scenarios.
The focus of this Special Issue is to outline the trends for the future, as what has been forgotten in the field of cardiac arrhythmias is often a patient-oriented, individualized approach; in fact, both optimizing shared decision making about arrhythmia treatment options and ensuring that patient values need to be taken into account are of great importance. In addition, it is now recommended and pursued that patient-reported outcomes are routinely collected to measure treatment success and improve patient care and the quality of healthcare. With greater emphasis on the need for lifestyle modifications and targeted therapy for intercurrent conditions, both the reduction of the AF burden and the improvement of outcomes are now possible and warranted.
It is our great privilege to invite you to contribute your work to this Special Issue on cardiac ablation. We ask that you provide your point of view or best results in terms of the individualized diagnosis and management of cardiac arrhythmias both in surgical and electrophysiological settings.
Dr. Mariusz Kowalewski
Prof. Dr. Piotr Suwalski
Guest Editors
Dear Colleagues,
Treatment of lipid metabolism disorders remains one of the foundations of preventive cardiology, affecting the populational life expectancy and quality. In recent years, owing to the hard work of multidisciplinary teams, we have acquired more resources in our therapeutic arsenal. Additionally, the entire spectrum of scientific research methodologies, including genetic studies, prospective epidemiologic cohort studies, Mendelian randomisation studies, and randomised trials of LDL-C lowering therapies, provided further insights to the impact of lipid profile on the burden of atherosclerotic disease and directly influenced the dynamic development of new therapeutic standards. With those advancements, as reflected in the current ESC 2019 guideline recommendations, patients at high and very high cardiovascular risk should now achieve more restrictive than ever before LDL-C treatment goals (≥50% reduction from baseline and <1.8 mmol/L [<70mg/dL]). On the other hand, many researchers also pursue the early introduction of dyslipidemia management in low-risk populations to reduce the LDL-C exposure and the concomitant atherosclerotic cardiovascular disease burden.
It is my great privilege to invite you to contribute to this Special Issue on cholesterol regulation. I welcome the submission of innovative original research, state-of-the-art reviews, and viewpoints dealing with the novel frontiers and individualized management of dyslipidemias
Dr. Michalina Kołodziejczak
Guest Editor
Manuscript Submission Information
Manuscripts should be submitted online at www.mdpi.com by registering and logging in to this website. Once you are registered, click here to go to the submission form. Manuscripts can be submitted until the deadline. All papers will be peer-reviewed. Accepted papers will be published continuously in the journal (as soon as accepted) and will be listed together on the special issue website. Research articles, review articles as well as short communications are invited. For planned papers, a title and short abstract (about 100 words) can be sent to the Editorial Office for announcement on this website.
Submitted manuscripts should not have been published previously, nor be under consideration for publication elsewhere (except conference proceedings papers). All manuscripts are thoroughly refereed through a single-blind peer-review process. A guide for authors and other relevant information for submission of manuscripts is available on the Instructions for Authors page. Journal of Clinical Medicine is an international peer-reviewed open access semimonthly journal published by MDPI.
Please visit the Instructions for Authors page before submitting a manuscript. The Article Processing Charge (APC) for publication in this open access journal is 2200 CHF (Swiss Francs). Submitted papers should be well formatted and use good English. Authors may use MDPI’s English editing service prior to publication or during author revisions.